Reendodontic retreatment with apical radicular perforation of tooth 11: academic scientific case report.
Abstract
Root perforation refers to a pathological communication between the root canal system and the external surface of the tooth. This complication may arise due to various factors, including extensive caries, root resorption, or inappropriate use of endodontic instruments. The choice of materials utilized during treatment is pivotal in effectively sealing the affected area. These materials should possess specific attributes, such as biocompatibility, sealing capacity, water solubility, non-cytotoxicity, and the ability to promote tissue repair and regeneration. Consequently, reparative bioceramic cements have been recognized as suitable agents for addressing this form of injury. The primary objective of this study is to present a clinical case report demonstrating the successful use of reparative bioceramic cement in sealing a root perforation during tooth 11's retreatment.
Introduction
Surgical accidents can pose significant challenges during endodontic therapy and may contribute to treatment failure. Various factors can predispose these accidents during root canal cleaning, including calcification, pulp nodules, malpositioned teeth in the dental arch, extensive caries, root resorption, and root perforations.
Root perforation is characterized by a communication between the root canal and the external surface of the tooth. This type of iatrogenic injury can lead to several consequences, ranging from chronic inflammation in the periodontium with granulation tissue to alveolar bone loss.
There is a range of materials available for the treatment of root perforations, such as amalgam, calcium hydroxide, glass ionomer, mineral trioxide aggregate (MTA), and bioceramic repair materials. MTA, containing tricalcium silicate, tricalcium aluminate, tricalcium oxide, and silicate oxide, is utilized not only for root perforations but also for direct pulp capping and retrograde filling. It offers several advantages, including bio-compatibility, bacteriostatic action, and good sealing capacity.
Bioceramic materials, as described by Raghavendra et al., are biocompatible repair cements known for their high sealing potential and antimicrobial properties. These materials, commonly used in dentistry, comprise calcium silicate, calcium phosphate, zircônia, and bioactive glasses, and are classified as calcium silicate-based cements or hydraulic calcium silicate cements.
Sousa et al. mention that these repair materials are synthesized through various chemical processes, which endows them with excellent biocompatibility and the ability to induce a regenerative response in tissues by absorbing osteoinductive substances during the bone healing process. They were introduced in dentistry primarily for repair and root canal obturation.
While no material possesses all the ideal properties for treating root perforations, bioceramic repair cements have gained significant popularity due to their excellent long-term sealing results. Thus, this study aims to demonstrate the successful sealing of a root perforation with bioceramic repair cement during the retreatment of endodontic therapy in tooth 11 through the presentation of a clinical case.
Case description
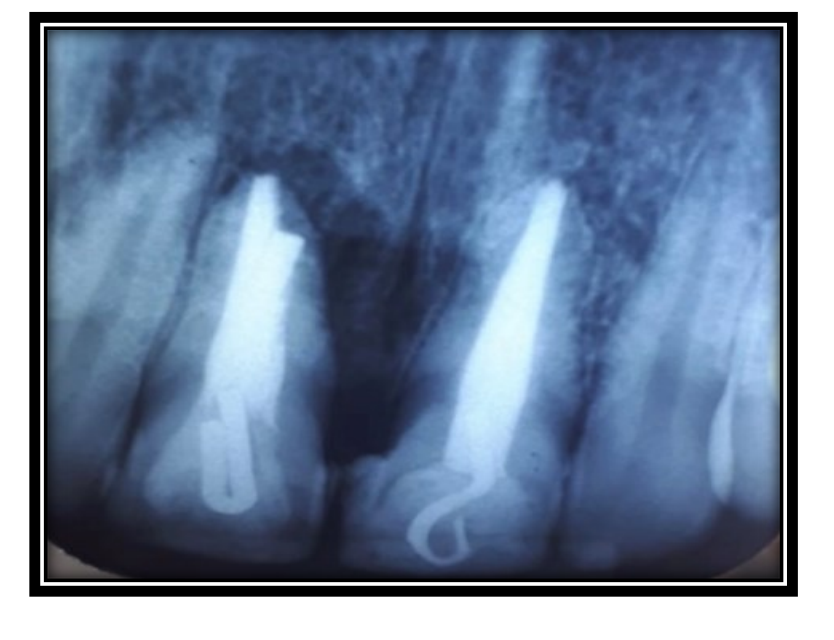
Patient MFBN, a 42-year-old female with melanoderma, sought treatment at the dental clinic of a Dentistry college located in the Ceará, reporting a history of trauma to tooth 11 with previous endodontic intervention. The intraoral clinical examination revealed darkening of the tooth, accompanied by edema and exudation (Figure 1). Subsequent periapical radiographic assessment revealed periapical radiolucency suggestive of root perforation in the apical region (Figure 2). To confirm the diagnosis of apical root perforation, a tomographic examination was performed.

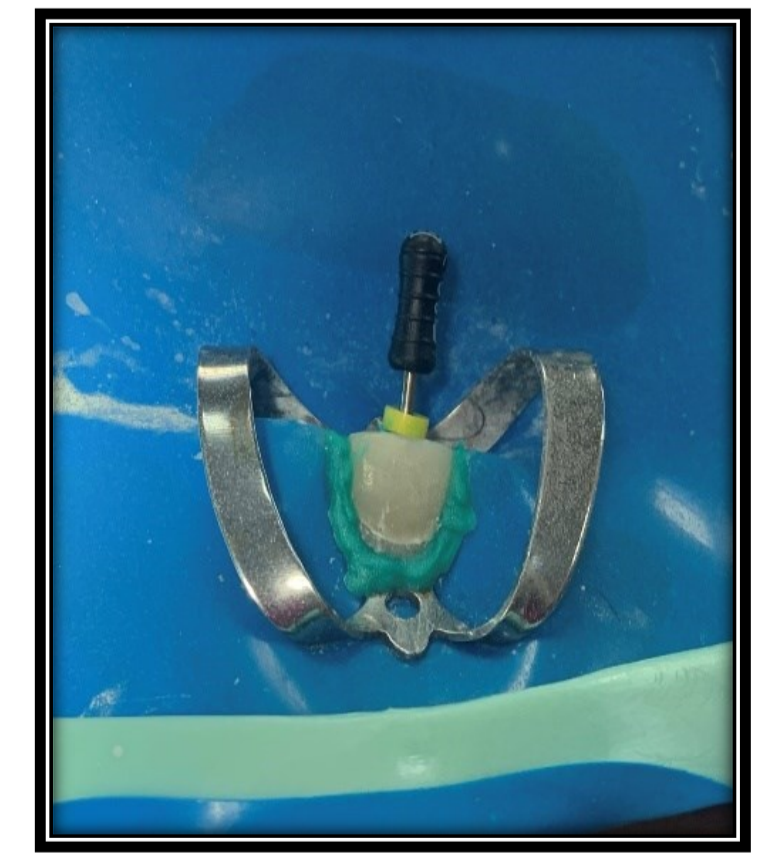
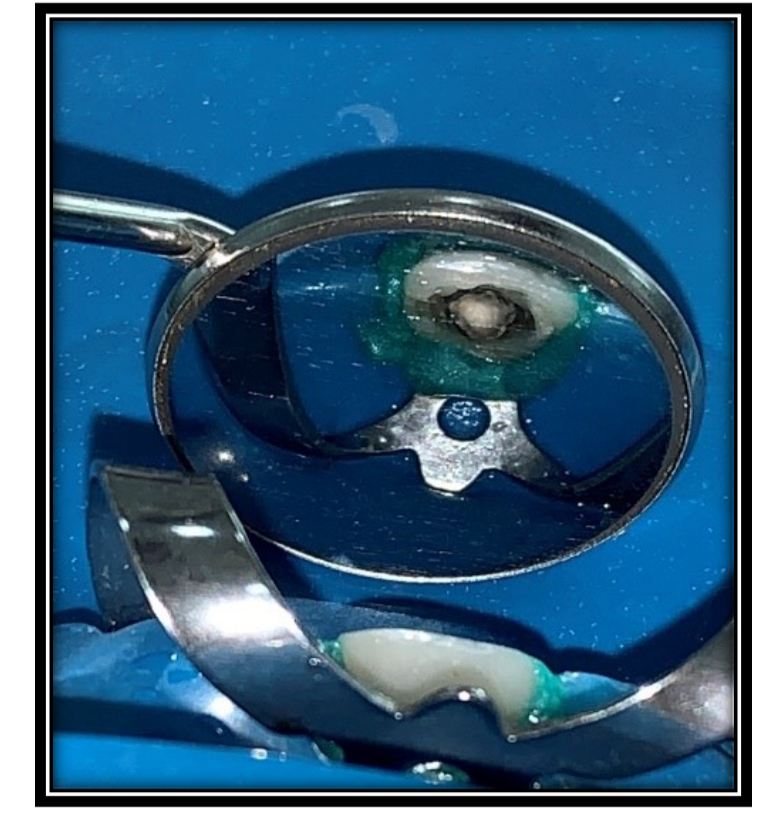
During the first treatment session, an infiltrative anesthesia of the anterior alveolar nerve was administered using 2% lidocaine with 1:100,000 epinephrine (DLF, Rio de Janeiro, Brazil) in tooth 11. Under rubber dam isolation, the clip employed as a fixed prosthesis retainer was removed using a diamond tip 1014 (KG-Sorensen, São Paulo, Brazil). The root canal was subsequently cleaned using a Reciproc R25 file and Clear Sonic ultrasonic insert (HELSE), aided by an electronic microscope, and abundant irrigation with 2.5% sodium hypochlorite (Figure 3).
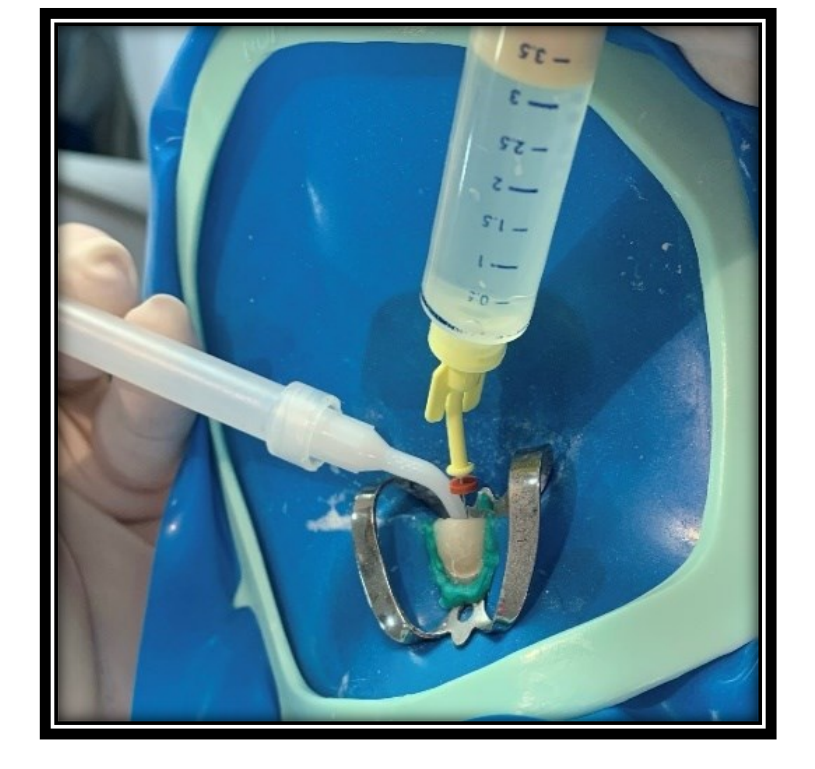
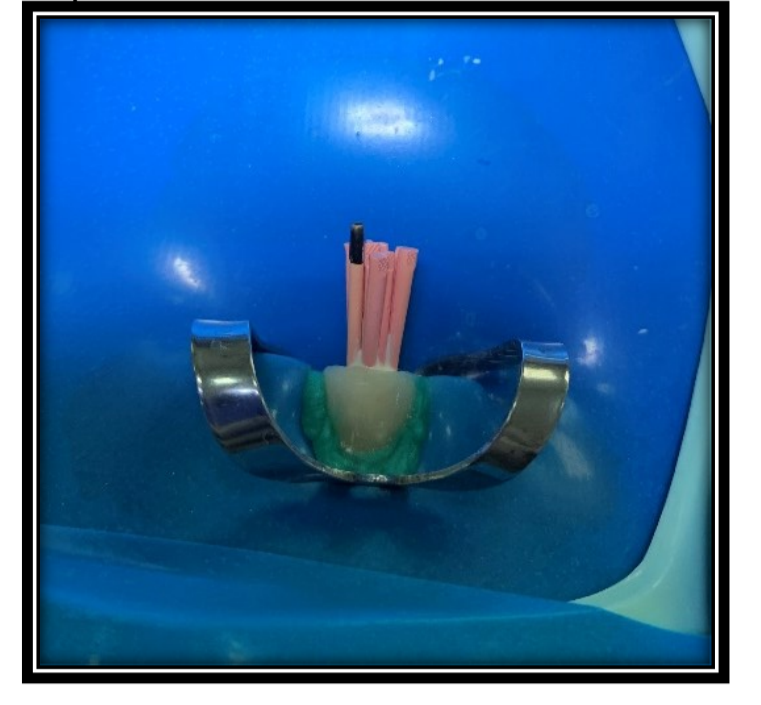
An 80 file was utilized to radiographically determine the working length (CRT) and perform root canal instrumentation (Figures 4 and 5). After biomechanical preparation, Bio-C Repair repair cement was carefully inserted at the site of the perforation using an absorbent paper point (Figure 6). Subsequently, the canal was filled with Calen plus PMCC, and a temporary restoration was applied. A follow-up periapical radiograph was taken to confirm the precise positioning of the repair cement within the perforation (Figure 7).
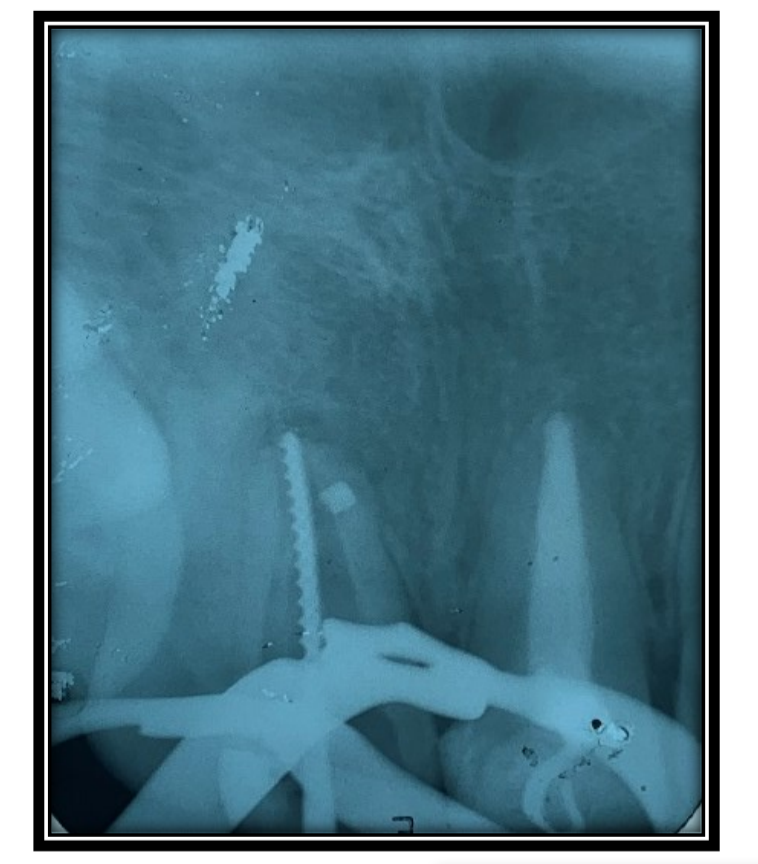

In the second treatment session, intracanal medication was removed using 2.5% sodium hypochlorite through Passive Ultrasonic Irrigation (PUI). Subsequent irrigation was carried out with EDTA and sodium hypochlorite, adhering to the final irrigation protocol. The canal was meticulously dried using capillary tips and absorbent paper cones (Figure 8). AH Plus sealer was employed for canal filling, and the warm vertical compaction technique was applied with the aid of McSpadden in low rotation (Figures 9 and 10). Finally, a radiograph was taken to verify the quality of the root canal filling (Figure 11).



Discussion
Root perforation represents a prevalent cause of operative accidents as highlighted by Alves et al.. It is characterized by an abnormal communication between the root canals and the periradicular tissues, arising from either pathological or iatrogenic factors.
Estrela et al. emphasize the significance of clinical findings and radiographic examinations for precise diagnosis and case planning. While periapical radiography is the commonly used imaging technique for diagnosing root perforation, it may lack specificity in complex cases. In this context, tomography offers a multitude of advantages over traditional radiography.
Electronic apex locators have proven valuable in diagnosing root perforations. An in vitro study by De Miranda Candeiro et al. evaluated three apical locators for their accuracy in locating simulated root perforations, demonstrating their efficiency in aiding the diagnosis of such complications.
The treatment of root perforations entails identifying the affected area, followed by decontamination and appropriate sealing with suitable materials. Prognosis tends to be less favorable when perforations are situated in the middle and apical thirds, in comparison to the cervical third and floor of the pulp chamber. Early treatment plays a crucial role in positively influencing the prognosis, making conventional therapy the preferred option for resolving such cases.
Sealing materials employed for root perforations should possess specific characteristics, including biocompatibility, non-cytotoxicity, radiopacity, bactericidal properties, hydrophilicity, dimensional stability, good sealing capacity, and the ability to prevent microleakage, as emphasized by. Mineral Trioxide Aggregate (MTA) has been widely used in perforation treatment due to its biocompatibility, excellent sealing ability, and tissue regenerative properties, resulting from its antimicrobial properties and alkaline pH (12.5). However, emerging reparative bioceramic cements offer numerous advantages for resolving complex root perforation cases.
Presently, reparative bioceramic cements are considered the gold standard for root perforation cases, displaying characteristics such as effective sealing capacity, excellent tolerance by periodontal tissues, and the induction of bone repair. Their biocompatibility is conferred by their similarity to biological hydroxyapatite, as noted by Estrela et al. [8] and Brait et al. Despite their exceptional properties and advantages, limited utilization is attributed to the high cost of commercially available materials.
This study employed Bio-C Repair (Angelus), a reparative bioceramic, which demonstrated favorable results in treating intraosseous root perforations, showcasing its excellent biocompatibility, capacity to induce bone repair, and clinical convenience.
Conclusions
In conclusion, the application of reparative bioceramic cements, in conjunction with a robust chemical-mechanical protocol, proves effective in treating root perforations. The use of Bio-C Repair fosters the recovery of periradicular tissues, thereby facilitating the functional restoration of the affected tooth.
Andressa C. F. de Brito, Clara I. A. S. e Silva, Alyssa M. Pinheiro, Irvina C. F. Melo, Ana B. H. R. D. de Sampaio, Eliane M. G. M. de Vasconcelo, Mario F. de P. Leonardi, Cicero L. G. Ramalho
References
- Estrela, C.; et al. Root perforations: a review of diagnosis, prognosis, and materials. Brazilian oral research, 2018, v. 32, p. 1-15.
- Alzahrani, O.; Alghamdi, F. Nonsurgical Management of Apical Root Perforation Using Mineral Trioxide Aggregate. Case reports in dentistry, 2021, v. 2021, p. 1-5.
- Alves, R.A.A.; et al. A Conservative Approach to Surgical Management of Root Canal Perforation. Case reports in dentistry, 2021, v. 2021, p. 1-6. 51, n. 3 Suppl 1, p. S128.
- Sousa, A.S.; Lima, H.M.; Salomão, M.B. CIMENTOS MTA E BIOCERAMICOS: REVISÃO DE LITERATURA. Revista Cathedral, 2020, v. 2, n. 3, p. 64-74.
- Costa, G.C. Agregado de Trióxido mineral: propriedades físicas, químicas, biológicas e seu uso como material selador em casos de perfuração radicular: revisão de literatura. 2021.
- de Miranda Candeiro, G.T.; et al. Tratamento de Perfuração Radicular Cervical com o uso de MTA-relato de caso. Research, Society and Development, 2022, v. 11, n. 2, p. e8911225474-e8911225474.
- de França, G.M.; et al. Uso dos biocerâmicos na endodontia: revisão de literatura. Revista de Ciências da Saúde Nova Es- perança, 2019, v. 17, n. 2, p. 45-55.
- Braitt, A.H.; et al. Selamento de perfuração com técnica de inserção modificada do MTA: relato de caso clínico. Rev. Odontol. Araçatuba (Online), 2022, p. 18-23.
- Arantes, E.A.; Boer, N.C.P. MATERIAIS USADOS NOS TRATAMENTOS DAS PERFURAÇÕES RADICULARES: REVISÃO DA LITERATURA. Revista Ibero-Americana de Humanidades, Ciências e Educação, 2022, v. 8, n. 5, p. 567-576.
- de Oliveira Resende, F.; et al. Tratamento com MTA Repair HP de extensa perfuração radicular após iatrogenia: relato de caso. Revista da Faculdade de Odontologia-UPF, 2019, v. 24, n. 1, p. 120-126.
- Fehlberg, B.K.; Bittencourt, G. Parendodontic surgery—apicoectomy and simultaneous obturation of root canals with mineral trioxide aggregate (MTA): case report. Dental Press Endodontics, 2019, v. 9, n. 1, p. 48-57.
- Raghavendra, S.S.; et al. Bioceramics in endodontics–a review. Journal of Istanbul University Faculty of Dentistry, 2017, v.
